What is a sling procedure for male stress urinary incontinence?
This relatively new technique uses a special plastic mesh to help support and reposition the urethra near the area of the urinary sphincter. It is a relatively straightforward procedure and is not a big operation.
Why do I need a male sling?
Insertion of a Male Sling is usually indicated for persistent mild or moderate urinary incontinence (involuntary urine leakage) after surgical removal of a malignant prostate gland (radical prostatectomy).
What is a male sling?
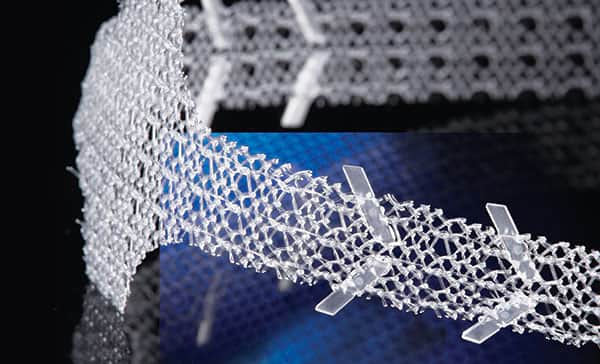
A Male Sling is a ribbon of mesh made out of a plastic material. It is surgically implanted under the urethra (water pipe). The sling pulls the water pipe upwards and supports it so that urine leakage is prevented.
The operation does not require major surgery and the recovery time is usually very quick. You will probably stay in hospital for one night.
Is this procedure right for me?
The Male Sling procedure has not been around for as long as other operations such as the Artificial Sphincter operation and so we don’t have as much information about results in the long term (e.g. more than 5 years). The success rate for this procedure is good (70-80%) but it may not be right for all patients.
Patients having this procedure should ideally have the following:
- Stress incontinence following radical prostatectomy operation.
- Failure to improve with pelvic floor exercises (for 6-12 months).
- Incontinence requiring 1 to 3 pads per day.
- No overnight incontinence.
- No radiotherapy treatment.
What are the alternatives to this procedure?
Alternatives to this procedure include incontinence into a pad, a permanent catheter, or insertion of an artificial urinary sphincter device.
What should I expect before the procedure?
You will usually be admitted to hospital on the same day as your surgery.
You will be asked not to eat and drink for six hours before surgery.
Immediately before the operation, the anaesthetist may give you a pre-medication, which will make you dry-mouthed and pleasantly sleepy.
You will be fitted with elasticated stockings to prevent venous thrombosis (clots in your legs).
Please inform your surgeon (before your surgery) if you have any of the following:
- An artificial heart valve.
- A coronary artery stent.
- A heart pacemaker or defibrillator.
- An artificial joint.
- An artificial blood-vessel graft.
- A neurosurgical shunt.
- Any other implanted foreign body.
- A regular prescription for a blood thinner e.g. Warfarin, Coumadin Xarelto®, Pradaxa®, Clopidogrel (Plavix®), Brilinta®, or Aspirin.
- Previous or current infection with an antibiotic resistant organism such as MRSA, VRE, etc.
What happens during the procedure?
A full general anaesthetic is normally used and you will be asleep throughout the procedure. You will usually be given an injection of antibiotics before the procedure, after you have been checked for any allergies. The anaesthetist may also use an epidural or spinal anaesthetic to reduce the level of pain afterwards.
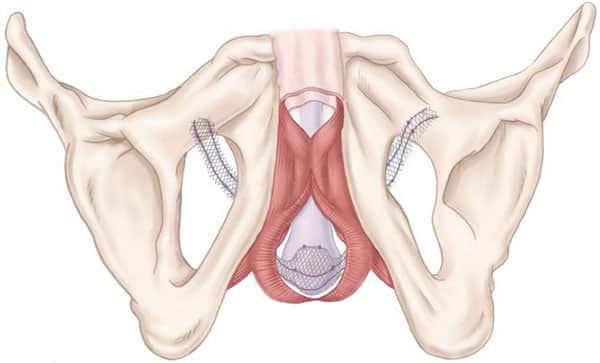
The surgeon will make a small incision in the area between the scrotum and the anus (perineum) and two further small incisions, one in each groin crease. The sling will be inserted through the perineum and passed upwards on each side into the incisions on your thighs (pictured). A catheter will be put in the bladder at the end of the procedure.
What happens immediately after the procedure?
You will be given fluids to drink at an early stage after the operation. You will be encouraged to mobilise as soon as you are comfortable to prevent blood clots forming in your legs and you will be given intravenous antibiotics. Your catheter will normally be removed before you go home. The average hospital stay is one day.
Are there any side-effects?
Most procedures are straightforward; however as with any surgical procedure there is a chance of side effects or complications.
Common (greater than 1 in 10)
- Burning or sting on urination.
- Urinary retention (inability to pass urine) requiring reinsertion of a catheter.
- Temporary perineal pain.
Occasional (between 1 in 10 and 1 in 50)
- Wound infection.
- Overactive bladder symptoms (frequency and urgency of passing urine).
Rare (less than 1 in 50)
Erosion of the sling into the urethra, which will require the sling to be surgically removed.
Bone infection.
What should I expect when I get home?
Pain
Your discomfort should disappear gradually over a few days although you may continue to feel tired for at least 10 to 14 days. Mild painkillers such as Paracetamol should be enough to deal with any pain.
Bowels
It is important that you do not get constipated. There are no dietary restrictions but you should try and eat plenty of fruit and vegetables and wholemeal bread. If you feel that you may be constipated, see your GP.
Exercise
You should take it easy for 6 weeks, although it is important to take some gentle exercise like walking, as you will be at a slight risk of developing a blood clot in your legs if you do not keep mobile.
During the first 6 weeks you should not:
- Bend over or squat.
- Lift or move heavy objects
- Dig the garden.
- Housework.
- Carry shopping.
It is safe to resume normal sexual activity 2 weeks after your surgery.
What else should I look out for?
If you develop a fever, severe pain on passing urine, inability to pass urine or worsening bleeding, you should contact your Surgeon immediately. If out of hours, please go to your nearest emergency department.
Disclaimer
This information is intended as a general educational guide and may not apply to your situation. You must not rely on this information as an alternative to consultation with your urologist or other health professional.
Not all potential complications are listed, and you must talk to your urologist about the complications specific to your situation.