Ultrasound-guided prostate biopsy is a day surgery procedure, used to obtain tiny samples of tissue from your prostate that can then be sent to the pathology laboratory for analysis under a microscope. The pathologist can check whether cancer is present. You may be recommended for biopsy, on the basis of your PSA level, if your prostate feels abnormal on a digital rectal examination (DRE), or your prostate looks abnormal on an MRI scan.
What does the procedure involve?
This procedure involves using an ultrasound probe, inserted via the back passage, to scan the prostate. Multiple biopsies are taken from the prostate, using a needle is inserted into the prostate through the probe.
What are the alternatives to this procedure?
Alternatives to this procedure include:
- Observation with repeat blood tests but without biopsies.
- Prostate MRI scan. A biopsy will still be required if an abnormality is found on an MRI scan. Also, a normal MRI does not exclude a significant cancer. An MRI scan can help improve the accuracy of a prostate biopsy by showing abnormal areas to target. There is no Medicare funding so the test can be expensive.
What should I expect before the procedure?
- If you are taking blood thinning medication such as aspirin, Plavix, Iscover, Assasantin, or warfarin, or supplements such as fish oils tablets please tell Dr Nathan at least 10 days before the procedure, as these may need to be discontinued to prevent postoperative bleeding.
- You will usually be given an antibiotic: noroxin or trimethoprim tablets to start one day before the biopsy, as well as an intravenous antibiotic when you are admitted to the hospital. If you have allergies to any antibiotics please let Dr Nathan now before the procedure.
- If you are having a sedation or a general anaesthetic do not have anything to eat or drink for 6 hours before your biopsy except for plain water which you can drink up to 4 hours before your procedure. Continue to take your normal medications unless advised not to. If you are not having sedation or a general anaesthetic, or only a local anaesthetic injection you can continue to eat and drink as normal.
Please arrive at the hospital at least 2 hours before the start of the theatre list so that the anaesthetist can see you and you can have an enema clear the rectum.
What happens during the procedure?
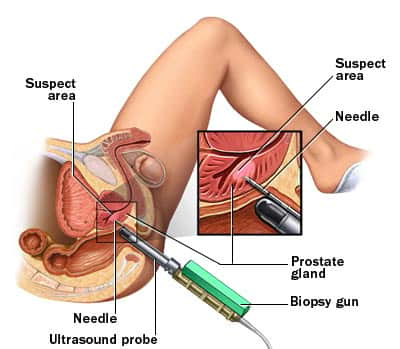
Using ultrasound for guidance, a fine, automated needle is inserted into the back passage until it reaches the prostate (shown in the diagram on the below). The test is not too painful (not much worse than a visit to the dentist), but you may feel a sharp needle prick as 6–12 tissue samples are taken, even if a local anaesthetic has been used. Alternately the procedure can be performed under sedation or general anaesthetic so that you will be unconscious so unaware of the procedure. Post-operative discomfort if any is usually mild and can be controlled with paracetamol. The results should be available within a few days. Remember, though, that biopsies of the prostate are only tiny samples of the whole gland, so small cancers may sometimes be missed. If the PSA continues to rise in spite of a negative biopsy result a further set of biopsies may be required. Several studies have shown that after 3 sets of negative biopsies prostate cancer is unusual because the rise in PSA that triggered the biopsy is usually the result of benign prostatic hyperplasia (BPH).
There is no evidence that biopsies cause prostate cancer to spread. The ability to spread (to metastasise) to other parts of the body, such as the skeleton, depends on the characteristics of the cancer cells themselves and tends to occur quite late in the disease.
Are there any side-effects?
Most procedures are straightforward. Although the complications listed below are well recognised, most patients do not suffer any problems.
Common (greater than 1 in 10)
- Blood in your urine.
- Blood in your semen for up to 6 weeks; this poses no problem for you or your sexual partner.
- Blood in your stools.
- Discomfort from the prostate due to bruising.
- Failure to detect a significant cancer of the prostate (10-20%). The procedure may need to be repeated if the biopsies are inconclusive or your PSA level rises further. Having an MRI scan before your biopsy may help reduce this risk and can help avoid a biopsy altogether in some men.
Occasional (between 1 in 10 and 1 in 50)
- Urinary tract infection.
- Blood infection (septicaemia) needing hospital admission (2% risk).
Haemorrhage (bleeding) needing admission (1% risk).
Rare (less than 1 in 50)
- Inability to pass urine (retention of urine) necessitating a temporary catheter.
What happens after the procedure?
You will be allowed home a few hours after your biopsy once you have recovered from your anaesthetic and passing urine. You cannot drive for 24 hours after an anaesthetic so please arrange for someone to pick you up from the hospital and look after you for 24 hours until the effects of the anaesthetic have worn off.
Continue taking the prescribed antibiotic tablets for a few days after the biopsy.
For several weeks after the procedure, you may notice small amounts of blood in your urine, semen and/or bowel motions. This is quite normal, but if you have any worries, consults your local doctor or Dr Nathan’s rooms. If you have heavy bleeding from your back passage, feel faint or unwell seek immediate medical attention.
Rarely may you have difficulty passing urine due to swelling of the prostate. If you are unable to pass urine and become uncomfortable a catheter (fine tube) may need to be inserted into your bladder and left for a few days until the swelling settles.
Urinary infections can occasionally occur as a consequence of the biopsy – if you feel a burning sensation on urination, notice that your urine is cloudy and/or smelly, find that you have to urinate more frequently than normal and/or you develop a temperature, have shaking attacks and feel generally unwell, contact your GP or urologist. He will probably prescribe more antibiotics or, very occasionally, admit you to hospital for treatment using an intravenous drip.
Arrange an appointment with your Urologist to discuss the results of your biopsy.
Disclaimer
This information is intended as a general educational guide and may not apply to your situation. You must not rely on this information as an alternative to consultation with your urologist or other health professional.
Not all potential complications are listed, and you must talk to your urologist about the complications specific to your situation.