What is the Prostate?
The prostate is one of the male sex glands. The prostate adds nutrients and fluid to the sperm. During ejaculation, the prostate secretes fluid that is part of the semen. The other major sex glands in men are the testes and the seminal vesicles. Together, these glands store and secrete the fluids that make up semen. The prostate is about the size of a walnut and can be divided into two parts referred to as the right or left lobes. It lies just below the urinary bladder and surrounds the upper part of the urethra. The urethra is the tube that carries urine from the bladder and semen from the sex glands out through the penis. As one of a man’s sex glands, the prostate is affected by male sex hormones. These hormones stimulate the activity of the prostate and the replacement of prostate cells as they wear out. The chief male hormone is testosterone, which is produced almost entirely by the testes.
What is cancer?
Our bodies are made up of cells; each cell can divide to make two new cells. Sometimes the process of cell division goes wrong and the cell continues to divide in an uncontrolled way, causing a cancer to develop which untreated can eventually spread to other parts of the body. I have recently found out that you have a cancer in the prostate, and have recommended that you have an operation called a radical Retropubic prostatectomy. This means that your prostate will be removed, in order to try and cure you of your cancer.
What is a Radical Retropubic Prostatectomy?
Radical prostatectomy means removing the entire prostate gland. Retropubic refers to the surgical approach by which this is performed – through an 8-10cm incision in the lower abdomen. The operation also removes the seminal vesicles. I will make every attempt to preserve the nerves that run next to the prostate which help to produce erections. However, these may have to be sacrificed in order to remove all of the prostate cancer. I may also elect to remove the lymph glands draining the prostate – I will discuss this with you before the operation.
What are the benefits of having a Radical Retropubic Prostatectomy?
If left alone prostate cancer can grow and invade surrounding structures e.g. bowel and bladder, or even spread to other parts of the body e.g. lymph glands and bones. Once the cancer has spread outside the prostate it is incurable. The operation aims to remove all of the cancer before it has a chance to spread outside the prostate.
What are the risks, consequences and alternatives associated with having a Radical Retropubic Prostatectomy?
As a sub-specialist in prostate cancer, you have been referred to me because I perform a lot of these operations (approximately 50/year). Most operations are straightforward; however as with any major surgical procedure there is a chance of side effects or complications.
Serious or frequently occurring risks
Frequent
- Erectile dysfunction (difficulty in achieving and maintaining and erection): 20 to 100% risk depending on age, level of sexual function prior to surgery, and whether one or both nerves can be spared which is related to the extent of cancer. Sexual function can take 12 months or more to recover after surgery. Please discuss your individual risk with Dr Nathan.
Occasional
- Temporary insertion of a bladder catheter and a wound drain.
- Dry orgasm with no seminal fluid produced causing infertility.
- Blood loss requiring transfusion or very rarely repeat surgery.
- Urinary incontinence, temporary or permanent, requiring protective pads or further surgery.
- Discovery that cancer cells have already escaped outside the prostate, needing observation or further treatment including radiotherapy or hormonal therapy.
- Scarring and stricturing of the join between the bladder and urethra, causing a blockage to the flow of urine, and the need for further endoscopic surgery to relieve the blockage.
- Delayed healing of the joint between the bladder and urethra (anastomosis) requiring your drain and catheter to remain for a longer period of time.
- Some men report a penile shortening of about 1-2cm. Sometimes this may be accompanied by a bent erection (Peyronie’s disease).
Rare
- Infection or hernia of incision requiring further treatment.
- Anaesthetic or cardiovascular problems possibly requiring intensive care admission (including chest infection, pulmonary embolus, stroke, deep vein thrombosis, heart attack and death).
- Rectal injury, very rarely needing temporary colostomy.
- It is important to discuss with me exactly what is going to happen during the operation. If you are concerned about any of these risks, or have further queries, please speak with me directly about them.
Alternatives to having a Radical Retropubic Prostatectomy
- Active Surveillance – monitoring the PSA level and repeating the biopsy at intervals.
- Radiotherapy – giving radiation treatment to the prostate.
- Brachytherapy – the implantation of radioactive seeds into the prostate.
- Hormonal therapy – for palliation of advanced disease.
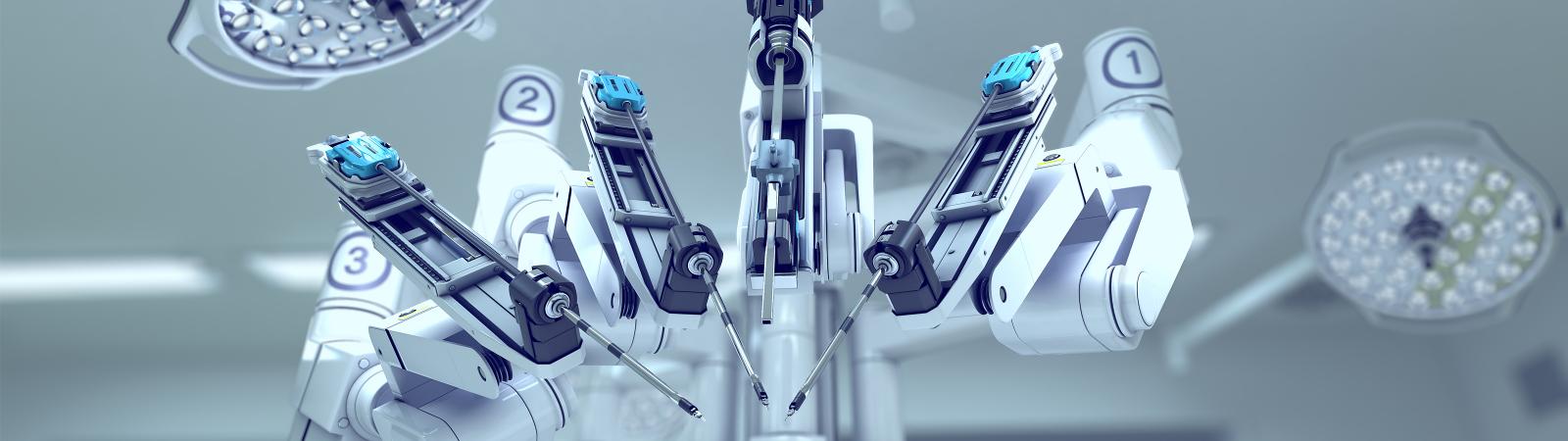
- Perineal, laparoscopic or robotic removal of the prostate I will discuss these alternatives with you.
Getting ready for the operation
Surgery is usually delayed for around 6 weeks after your biopsy to allow inflammation to settle- this makes it easier to release the erectile nerves from the prostate during surgery.
If you smoke, try and cut down or preferably stop, as this reduces the risks of heart and chest complications during and after the operation. If you do not exercise regularly, try and do so for at least half an hour per day e.g. brisk walk or swimming. If you are over weight try to get in better shape.
It is also recommended that you perform pelvic floor exercises regularly for 1 month before your surgery to speed up your return to full continence after the operation. If you are not sure about how to do this referral to a physiotherapist can be arranged.
If you are on medication to thin the blood such as warfarin, aspirin, plavix, iscover, or supplements such as fish oils please let Dr Nathan know at least 10 days before surgery as these medications may need to be discontinued to prevent excessive bleeding at the time of surgery. You can continue to take your other medications as normal.
Talk to your anaesthetist (my receptionist will give you his/her details) and discuss your anaesthetic and pain relief.
Before the operation you will be asked to sign a consent form. It is important that you read this patient information leaflet and have had adequate discussions about the implications of radical prostatectomy with Dr Nathan before signing your consent form.
You will be given a form from Dr Nathan’s rooms to perform routine blood tests, and a urine test a few days before your operation.
The day before your admission you can eat a light diet until 8pm (avoid deep fired foods, red meat or pasta). Avoid getting dehydrated. You can continue to drink clear fluids until midnight then nil by mouth after that. You will be admitted to hospital on the morning of surgery. If your operation is in the afternoon you can drink sips of plain water only in the morning up to 4 hours before your surgery (no later than 9am). You will be prescribed 2 enemas, one to be taken at home 4-8hours before surgery, and the other as soon as you are admitted to hospital on the morning of surgery. The enemas help to clear the rectum and prevent rectal injury during the operation.
Precautions will be taken to stop you developing a blood clot; you will be asked to wear elasticated support stockings and will be given injections of blood thinning drugs after your operation.
The morning of your operation you should have a bath or a shower. You will be given a theatre gown to wear before you go down to theatre. A nurse or porter will take you to the operating theatre reception, your details will be checked and you will go through to the anaesthetic room.
What sort of anaesthetic will I have?
The anaesthetist will visit you before the operation to discuss this with you. This operation is performed under a general anaesthetic. This means that you will be fully asleep during the operation.
What should I expect after the operation?
After your operation you will normally go back to the surgical ward. Occasionally patients go to the High Dependency Unit for 24 hours where the doctors and nurses can monitor you more closely. The purpose of your stay here is to monitor your blood pressure, heart rate and fluid levels using accurate equipment. You will be given oxygen through a mask or nasal tube; this is to aid your recovery.
The physiotherapist will visit you and discuss your progress after the operation including breathing and leg exercises, walking and stairs.
Pain
Pain from this operation can be easily controlled. Different methods of pain control are available, and include epidural analgesia and patient controlled analgesia. Your anaesthetist will explain the advantages and disadvantages of these to you. If you are experiencing any pain it is important to tell the nurses so that they can adjust your medication to control this. Usually after a couple of days the pain has lessened so it can be controlled using tablets alone.
Eating and drinking
You can start drinking small amounts of clear fluid immediately after your surgery. You will also have a drip, which will give you any extra fluids that you need. If you feel sick you are advised not to drink until this feeling has passed. You will be offered medication if the feeling doesn’t go away. You should be able to start eating the day after your surgery.
Wound drains
You will have one or two flexible tubes coming out of your abdomen, near to the wound; their purpose is to drain away any fluids collecting underneath your wound. The tube is connected to a bag or bottle. When the amount of fluid coming from the tube has slowed down to only a small amount I will advise the nurses to remove it.
Catheter
A urinary catheter is a tube that runs from the bladder out through the tip of the penis and drains into a bag. It is important to drain the urine in this way until the new connections that are made after removing the prostate have healed. The catheter stays in for 7-14 days so you usually go home with it still in. You will be admitted to hospital 10-14 days after your operation to have the catheter removed. Sometimes an x-ray test (cystogram) maybe performed to check that the internal join has healed before your catheter is removed. You will be given a date to come to have the catheter removed.
Do not let anyone remove the catheter before it is due to come out.
[Developer Note: Style the paragraph above using Foundation Panel]
How long will it take to recover?
Most patients stay in hospital for approximately 3-5 days. I will monitor your progress and decide when it is appropriate for you to go home.
Before you are allowed home:
- You must be eating and drinking normally.
- You must have had your bowels open.
- Mild painkillers such as Paracetamol and Voltaren must adequately control any pain.
- Your temperature must be normal.
- Your wound must be healing.
- 7-14 days after your operation, you will be re-admitted to hospital for removal of your catheter.
Discharge information and at home advice
Pain
Mild painkillers such as Paracetamol should be enough to deal with any pain.
Bowels
It is important that you do not get constipated. There are no dietary restrictions but you should keep well hydrated (3litres of fluid/day) and try to eat plenty of fruit and vegetables and wholemeal bread. If you feel that you may be constipated, see your GP. After the operation I advise patients to avoid enemas or suppositories for 6 weeks to avoid rectal injury.
Catheter
If you have any problems with your catheter, you should ring my rooms or the surgical ward for advice. It is very important that your catheter does not block or become dislodged.
DO NOT ALLOW ANYONE TO REMOVE YOUR CATHETER UNLESS YOU HAVE BEEN ADMITTED TO HOSPITAL
Exercise
You should take it easy for a month, although it is important to take some gentle exercise like walking, as you will be at a slight risk of developing a blood clot in your legs.
During the first 6 weeks you should not:
- Lift or move heavy objects.
- Dig the garden.
- Do housework.
- Carry shopping.
Work
Recovery takes 6-8 weeks from your operation date; I will be able to advise you when it will be safe to return to work as this depends on your occupation. My rooms can provide a sick note for your work.
Driving
You can resume driving 2-4 weeks after surgery once your catheter is out, if you are well, feel comfortable and do not require strong pain killers.
Sexual intercourse
The issue of resuming sexual function will have been discussed with you prior to your surgery as this type of operation affects sexual function. It is an issue that can be revisited post surgery when you feel that the time is right for you to do this. It is rare to get erections immediately after the catheter has been removed, and I may recommend trying some tablets (e.g. Viagra, Levitra, Cialis) in the early phase of recovery to improve the chances of attaining an erection.
Disclaimer
This information is intended as a general educational guide and may not apply to your situation. You must not rely on this information as an alternative to consultation with your urologist or other health professional.
Not all potential complications are listed, and you must talk to your urologist about the complications specific to your situation.