What does the procedure involve?
Removal of the obstructing portion of the prostate gland through an abdominal incision when the prostate gland is too big to remove using a telescope.
What are the alternatives to this procedure?
Alternatives to this procedure include drugs to shrink or relax the prostate, long-term catheter drainage, Holmium laser removal of the prostate and telescopic removal of prostate obstruction (TURP).
What should I expect before the procedure?
If you regularly take aspirin or clopidogrel, you must mention this to Dr Nathan because these drugs can cause increased bleeding after surgery. Stopping them may reduced the risk of bleeding but this can result in increased clotting, which may also carry a risk to your health. You will need to discuss the risks and benefits of the treatment with Dr Nathan
You will usually be admitted to hospital on the same day as your surgery. You may receive an appointment for a “pre-assessment” to assess your general fitness for anaesthesia.
Immediately before the operation, the anaesthetist may give you a pre-medication, which will make you dry-mouthed and pleasantly sleepy.
Please tell your DR Nathan (before your surgery) if you have any of the following:
- An artificial heart valve.
- A coronary artery stent.
- A heart pacemaker or defibrillator.
- An artificial joint.
- An artificial blood-vessel graft.
- A neurosurgical shunt.
- Any other implanted foreign body.
- A regular prescription for warfarin, aspirin or clopidogrel (Plavix®).
- A previous or current MRSA infection.
What happens during the procedure?
Either a full general anaesthetic (where you will be asleep) or a spinal anaesthetic (where you are unable to feel anything from the waist down) will be used. All methods reduce the level of pain afterwards. Your anaesthetist will explain the pros and cons of each type of anaesthetic to you. You will usually be given injectable antibiotics before the procedure, after checking for any allergies.
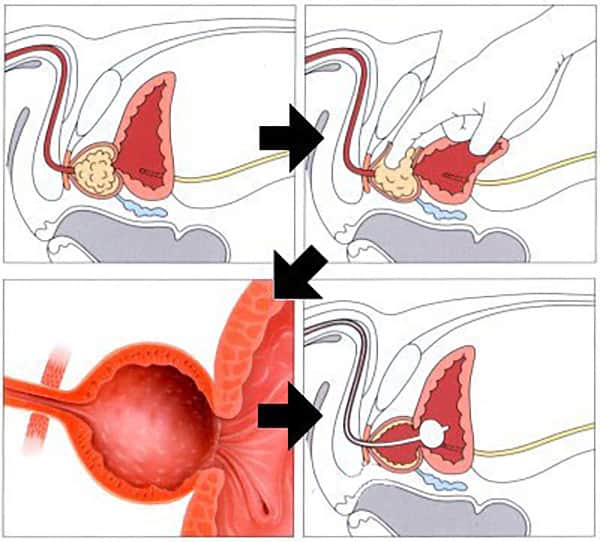
The operation is performed through an incision in the lower part of your tummy, after a telescope inspection of your bladder. The outer shell of the prostate gland is incised the central obstructing part of the prostate is removed by finger dissection (pictured). A bladder catheter and a drain are inserted at the end of the procedure. The procedure normally takes 45 to 60 minutes.
What happens immediately after the procedure?
You will have some bleeding from the prostate area after the operation but the urine usually clears of blood after 48 hours. Some patients, however, may lose more blood for longer. If the loss is large, you may require a blood transfusion to prevent you from becoming anaemic. You will be able to eat and drink the morning after the operation; this may be allowed earlier after a spinal anaesthetic. The wound drain is usually removed after two to four days and the catheter after four to six days, after which urine can be passed in the normal way. At first, you may get pain when passing urine and it may come more frequently than normal. Any discomfort can be relieved by tablets or injections and the frequent passage usually improves within a few days. It is not unusual for your urine to turn bloody again after catheter removal. Some patients cannot pass urine at all after the operation. If this happens, we normally pass another catheter to let the bladder recover before trying again without the catheter. The average hospital stay is seven days.
Are there any side-effects?
Most procedures have possible side-effects. But, although the complications listed below are well recognised, most patients do not suffer any problems.
- Common (greater than 1 in 10).
- No semen is produced during an orgasm.
- Passing urine frequently may remain after surgery.
- Bleeding requiring further surgery or transfusions (5%).
- 10% chance of impotence (poor erections).
- Scarring of the bladder neck producing similar symptoms to prostatic obstruction.
- Occasional (between 1 in 10 and 1 in 50).
- Finding of unsuspected cancer requiring further treatment.
- Infection, pain or hernia of incision requiring further treatment.
- Incontinence of urine (poor urinary control), which may be temporary or permanent (2 to 4%).
- Rare (less than 1 in 50).
- Anaesthetic or cardiovascular problems possibly requiring intensive care admission (including chest infection, pulmonary embolus, stroke, deep vein thrombosis, heart attack and death).
What should I expect when I get home?
It is advisable that you continue to wear your elasticated stockings for 14 days after you go home. It will be at least 14 days before full healing of the wound occurs and it may take up to six weeks before you recover fully from the surgery. You may return to work when you are comfortable enough and your GP is satisfied with your progress.
What else should I look out for?
If you develop a fever, severe pain when passing urine, you cannot pass urine or any bleeding gets worse, you should contact Dr Nathan’s rooms or attend your local emergency department out of hours. If you develop a temperature, increased redness, throbbing or drainage at the site of the operation, please contact Dr Nathan’s rooms or your GP.
One man in five experiences further bleeding 10 to 14 days after getting home; this is due to scabs separating from the cavity of the prostate. If you increase your fluid intake, the bleeding should stop quickly. If it does not, you should contact Dr Nathan’s rooms or your GP who will prescribe some antibiotics for you. In the event of severe bleeding, passage of clots or sudden difficulty in passing urine, you should contact Dr Nathan’s rooms or attend your local emergency department out of hours, because it may be necessary for you to be re-admitted to hospital.
Are there any other important points?
Removal of your prostate should not adversely affect your sex life provided you get normal erections. You may have sex as soon as you are comfortable, usually after three to four weeks.
You should start pelvic floor exercises as soon as possible after the operation because they improve your control when you get home. If you need any specific information on these exercises, please contact the ward staff or your urologist’s rooms. The symptoms of an overactive bladder may take three months to resolve whereas the flow is improved immediately.
You and your GP will be informed of your biopsy results as occasionally we may find unexpected cancer.
Disclaimer
This information is intended as a general educational guide and may not apply to your situation. You must not rely on this information as an alternative to consultation with your urologist or other health professional.
Not all potential complications are listed, and you must talk to your urologist about the complications specific to your situation.