What does the procedure involve?
Orchidectomy is the surgical removal of one or both testicles. The reason is for the treatment of testicular cancer. Removal of the testis via a groin incision for suspected testicular cancer. A testicular implant may be inserted at the same time if you wish
What are the alternatives to this procedure?
There are usually not alternatives to this procedure but, sometimes, the surgeon may agree to observation, biopsy or partial removal of the testis where a suspected tumour is present. This, however, is very uncommon.
What should I expect before the procedure?
Having only one testis should not adversely affect your life because the remaining testicle takes over its function. Your sex life and ability to father children should be unchanged. However, testicular cancer and its treatments (especially chemotherapy) can affect fertility. You will, therefore, be given the opportunity to produce semen samples for storage. These can be used in the future for assisted conception if your fertility does not recover after treatment. If you are concerned about the cosmetic results of losing a testicle, we can insert a false testicle (prosthesis) during the operation.
You will usually be admitted to hospital on the same day as your surgery.
You will be asked not to eat and drink for six hours before surgery.
Immediately before the operation, the anaesthetist may give you a pre-medication, which will make you dry-mouthed and pleasantly sleepy.
Please tell your surgeon (before your surgery) if you have any of the following:
- An artificial heart valve.
- A coronary artery stent.
- A heart pacemaker or defibrillator.
- An artificial joint.
- An artificial blood-vessel graft.
- A neurosurgical shunt.
- Any other implanted foreign body.
- A regular prescription for a blood thinner e.g. Warfarin, Coumadin Xarelto®, Pradaxa®, Clopidogrel (Plavix®), Brilinta®, or Aspirin.
- Previous or current infection with an antibiotic resistant organism such as MRSA, VRE, etc.
What happens during the procedure?
Either a full general anaesthetic (where you will be asleep) or a spinal anaesthetic (where you are unable to feel anything from the waist down) will be used. All methods reduce the level of pain afterwards. Your anaesthetist will explain the pros and cons of each type of anaesthetic to you.
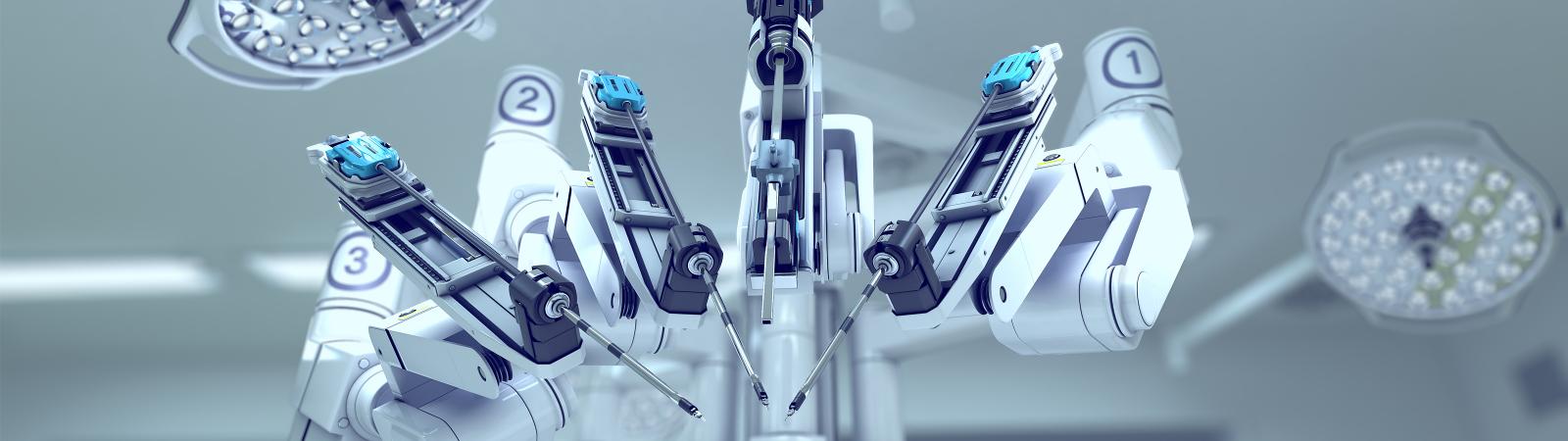
We normally remove your testicle through an incision in the groin (pictured). It may be necessary to take biopsies from the other (normal) testis. If this is needed, it will be discussed with you before the procedure. The operation takes approximately 30 minutes.
What happens immediately after the procedure?
You may eat, drink and mobilise as soon you have fully recovered from the anaesthetic. You will be able to leave hospital as soon as you are comfortable. This will depend on your having someone who can take you home and remain with you for the first 24 hours after discharge. The average hospital stay is one to two days.
Are there any side-effects?
Most procedures are straightforward but as with any operation there are potential complications and side-effects.
Common (greater than 1 in 10)
- Cancer, if found, may not be cured by removal of the testis alone.
- Additional procedures or treatments such as surgery, radiation or chemotherapy may be needed.
- We may need permission to biopsy the other testis if it is small, abnormal or has not descended properly.
Occasional (between 1 in 10 and 1 in 50)
- The pathology may not show no cancer.
- Microscopic examination of the removed testicle may not give a definite result.
- Infection of the incision needing further treatment. If a prosthesis has been inserted this may need to be removed.
- Bleeding needing further surgery.
- Loss of future fertility.
Rare (less than 1 in 50)
- Pain, infection or leaking needing removal of implant.
- Cosmetic appearance of the implant may not be acceptable.
- Implant often lies higher in the scrotum than normal testis.
- You may be able to feel a stitch at one end of the implant.
- Long-term risks from use of silicone products are not known.
What should I expect when I get home?
Your groin and scrotum may be uncomfortable for 7 to 10 days but simple painkillers will usually relieve this discomfort. It is common to notice some bruising in your groin and scrotal area. You may find it more comfortable to wear supportive pants rather than boxer shorts.
You may shower 24 hours after the procedure but make sure that your wound
is thoroughly dry afterwards. You should be able to return to work after two weeks but it is sensible to avoid heavy lifting and strenuous exercise for a month.
Sex can be resumed after two weeks although some men find the “stress” of surgery reduces their sex drive temporarily. Testicular cancer cells cannot be passed to your partner during sex.
Absorbable stitches are normally used but these may take up to 90 days to disappear completely.
What else should I look out for?
If you develop a temperature, increased redness, throbbing or drainage at the site of the operation, please contact your Surgeon or GP. In case of an emergency attend your nearest emergency department or call ‘000’.
Are there any other important points?
Please make sure you have a follow up appointment with your surgeon 1-2 weeks after your procedure. Further treatment will usually be carried out under the supervision of a specialist Oncologist.
Disclaimer
This information is intended as a general educational guide and may not apply to your situation. You must not rely on this information as an alternative to consultation with your urologist or other health professional.
Not all potential complications are listed, and you must talk to your urologist about the complications specific to your situation.