What does the procedure involve?
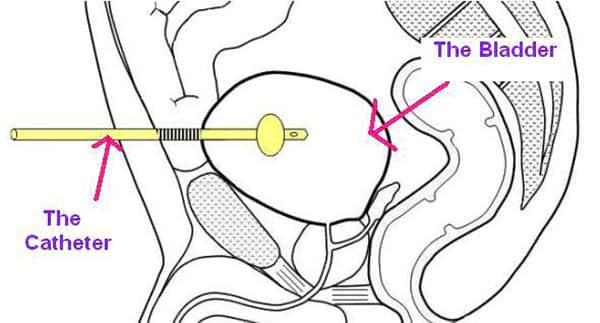
Placement of drainage tube into bladder through an incision in the skin over the bladder area (just above the pubic hairline). Cystoscopy (inspection of the bladder) is often performed to aid insertion of this tube.
There are many different reasons for insertion of a suprapubic catheter (SPC). The reason you are having this procedure will be discussed with you in detail prior to the operation.
SPC is a method for draining urine from the bladder that avoids the need for a catheter in the urethra. There is some evidence that the risk of long term or repeated bladder infections in slightly less if you have an SPC rather than a urethral catheter.
What are the alternatives to this procedure?
Alternatives to this procedure include a catheter through the urethra and permanent urinary diversion.
What should I expect before the procedure?
You will usually be admitted to hospital on the same day as your surgery.
You will be asked not to eat and drink for six hours before surgery. Immediately before the operation, the anaesthetist may give you a pre-medication, which will make you dry-mouthed and pleasantly sleepy.
Please tell your surgeon (before your surgery) if you have any of the following:
- An artificial heart valve.
- A coronary artery stent.
- A heart pacemaker or defibrillator.
- An artificial joint.
- An artificial blood-vessel graft.
- A neurosurgical shunt.
- Any other implanted foreign body.
- A regular prescription for warfarin, aspirin or clopidogrel (Plavix®).
- A previous or current MRSA infection.
What happens during the procedure?
Either a full general anaesthetic (where you will be asleep) or a spinal anaesthetic (where you are unable to feel anything from the waist down) will be used. All methods reduce the level of pain afterwards. Your anaesthetist will explain the pros and cons of each type of anaesthetic to you.
You will usually be given injectable antibiotics before the procedure, after checking for any allergies.
The surgeon will first fill your bladder with fluid and then insert your suprapubic through a small incision in your lower tummy (pictured), just above the pubic hairline. In patients with small bladders, the incision often needs to be larger so that the bladder can be seen clearly to allow the catheter to be inserted. Correct positioning within the bladder is checked by telescopic inspection of the bladder via the water pipe (urethra).
What happens immediately after the procedure?
The catheter may be stitched in place at first, but these stitches can be removed after a week or so, without the catheter falling out.
The average hospital stay is two days.
You will be shown how to care for the catheter. Most SPC need to be changed every six weeks (a simple, painless, five-minute procedure done in outpatients), and we like to perform the first change under supervision in the clinic/hospital.
Are there any side-effects?
All procedures have the potential for side-effects. Although these complications are well recognised, the majority of patients do not have problems after a procedure.
Risks of the anaesthetic need to be discussed with the anaesthetist who will be looking after you during the operation, and who will visit you beforehand.
There are specific risks with this surgical procedure, and these will be discussed with you before your procedure. As a guide to complement that one-on-one discussion with your surgeon, these include:
Common (greater than 1 in 10)
- Temporary mild burning or bleeding during urination.
Occasional (between 1 in 10 and 1 in 50)
- Infection of the bladder needing antibiotics (occasionally, recurrent infections).
- Blocking of the catheter needing unblocking.
- Bladder discomfort and pain.
- Persistent leakage from the water pipe (urethra), which may need a further operation to close the bladder neck.
- Development of stones and debris in the bladder, causing catheter blockage, and requiring removal or crushing by a further procedure.
Rare (less than 1 in 50)
- Bleeding requiring irrigation, or additional catheterisation, to remove blood clot.
- Rarely, damage to surrounding structures, such as bowel or blood vessels with serious consequences, possibly needing additional surgery.
What should I expect when I get home?
When you get home, you should drink twice as much fluid as you would normally for the first 24 to 48 hours. This helps to flush your system through and minimises any bleeding.
The catheter will need to be changed, for the first time, after approximately six weeks and we will arrange this for you in the outpatient clinic or hospital. Thereafter, further catheter changes can be performed by your GP or community nurse.
What else should I look out for?
If you develop a fever, redness in the wound, any pus from the catheter site or worsening bleeding, you should contact your GP or Surgeon immediately.
In the event of the catheter falling out, it must be replaced as a matter of urgency or the track will close up (often in a few hours) and it may not be possible to re-insert the catheter. Contact your GP for immediate advice or go directly to your local hospital Emergency Department to have a new catheter put back in before the track closes.
Are there any other important points?
Some discharge from the catheter site is not unusual in the longer term. If the catheter blocks within the first four weeks, the channel between the skin and the bladder will not have healed completely so it is not possible to change the catheter easily. In this event, it is important that the catheter is not taken out in an attempt to change it. It should simply be left in place and a urethral catheter inserted as well, followed by immediate notification of your Urologist.
Disclaimer
This information is intended as a general educational guide and may not apply to your situation. You must not rely on this information as an alternative to consultation with your urologist or other health professional.
Not all potential complications are listed, and you must talk to your urologist about the complications specific to your situation.